Electronic Health Record (EHR) systems are the backbone of modern healthcare data management. They store patient information digitally and streamline clinical workflows. Yet, not all EHR systems function the same way. With different infrastructure models, specialties, and accessibility features, healthcare organizations must understand the available options before committing to a system.
There are several types of EHR systems—each built to serve specific needs, practice sizes, and compliance requirements. From cloud-based platforms that offer easy access and scalability to on-premise systems that provide complete control, the choice impacts daily operations, cost, and security. This blog breaks down the major EHR system types to help providers make informed, practical decisions for their environment.
Cloud-based EHR systems are a modern solution for managing patient records online. Instead of storing data on computers or servers inside a hospital or clinic, these systems keep the information on remote servers, like how your email or photos might be saved in Google Drive or iCloud.
Here’s what that means in simple terms:
A cloud-based EHR system saves all patient information—like medical history, lab results, medications, and visit notes—on secure servers operated by an external service provider. Healthcare professionals can log in to the system using a web browser or mobile device to access the data from anywhere.
This differs from traditional systems that require you to be on-site at a hospital or clinic to view or update records.
Cloud-based EHRs are especially popular among small to mid-sized clinics for several reasons:
🔸 Low upfront costs: No need to buy expensive servers or hire a large IT team.
🔸 Easy setup and updates: The provider handles software updates, security patches, and maintenance.
🔸 Remote access: Doctors and staff can log in from any internet-connected device, useful for telemedicine or home visits.
🔸 Data backup and security: Most providers automatically back up the data and use encryption to keep it safe.
🔸 Scalability: Start with a small setup and expand as your practice grows.
🔸 Mobility: Access patient records on the go, ideal for traveling doctors or rural health workers.
🔸 Reduced IT burden: There is no need for a full-time IT department; the subscription often includes support.
When using a trusted provider, cloud-based EHRs follow HIPAA compliance standards to protect patient data. They include features like:
🔸 End-to-end encryption
🔸 Access controls and authentication
🔸 Regular backups and disaster recovery options
Still, providers must choose a vendor that outlines their security practices and compliance certifications.
A small dermatology clinic with limited space and budget can adopt a cloud-based EHR to manage patient appointments, record treatments, and access data remotely. They don’t need to worry about buying extra hardware or hiring a tech team; they can access records from home during off-hours.
Related Read: Choosing Between Ready-Made and Custom EHR Solutions
On-premise EHR systems are the traditional way of managing patient health records. All the software, servers, and data are stored and managed directly within the hospital or clinic building in this setup.
Think of it like having your private library. Every book (or, in this case, patient file) is stored on-site, and only people within the building can access it. You own it, manage it, and are fully responsible for it.
An on-premise EHR system is installed on servers at the healthcare facility. All the patient information—notes, lab reports, prescriptions—is stored on those local servers. Access is usually limited to computers within the clinic’s network, unless remote access is set up with additional configurations.
Unlike cloud-based systems, where a third party manages the server and software, the healthcare organization handles everything, from hardware maintenance to software updates.
These systems are generally used by:
🔸 Large hospitals
🔸 Multi-specialty clinics
🔸 Healthcare organizations with in-house IT teams
🔸 Institutions that require complete control over their data and systems
🔸 Full control: You have complete ownership of your data and how it’s stored.
🔸 Customizability: Easier to customize to fit specific workflows and needs.
🔸 Offline access: Since data is stored locally, the system can still work even if the internet goes down.
🔸 High upfront costs: You must invest in servers, software licenses, and IT staff.
🔸 Ongoing maintenance: You are responsible for security updates, backups, and hardware repairs.
🔸 Scalability issues: Expanding the system can be complex and costly compared to cloud options.
While you have total control over security, you carry the entire burden. Hospitals must:
🔸 Set up secure firewalls
🔸 Regularly update software
🔸 Back up data routinely
🔸 Train staff on cybersecurity
For organizations with the right resources, this setup can provide high security and customization.
A large hospital network with multiple departments and thousands of patient visits per day might choose an on-premise EHR system. With a full-time IT staff and strict internal policies, they can ensure the system aligns with their complex workflows and security protocols.
Related Read: Epic EHR Explained: How It Transforms Healthcare Operations and Patient Care
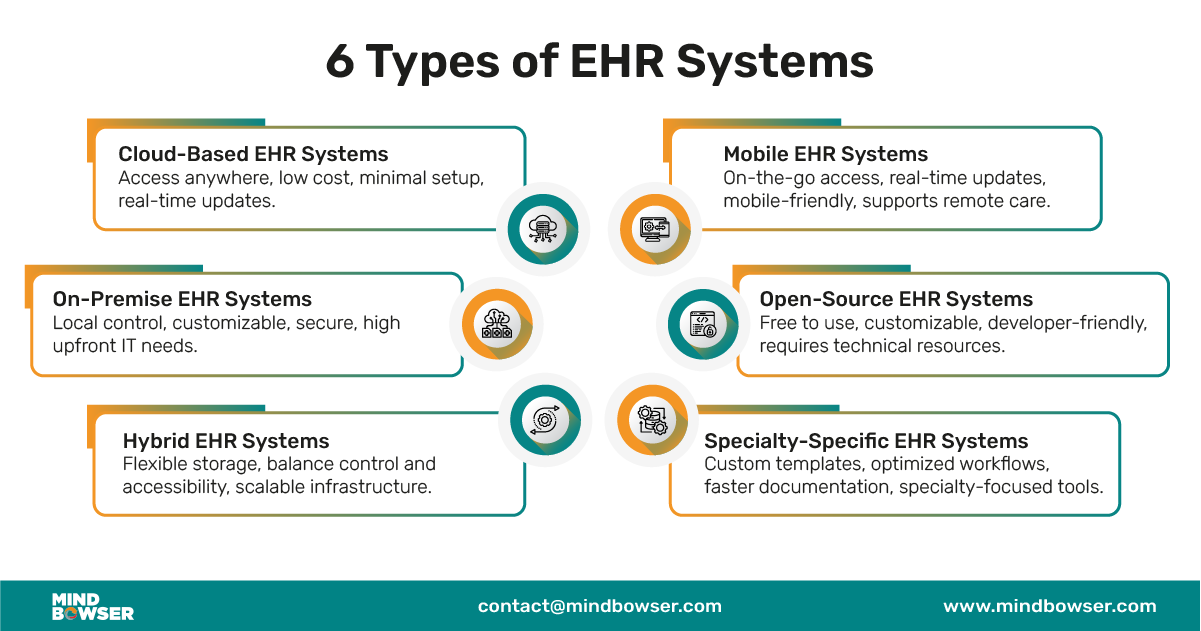
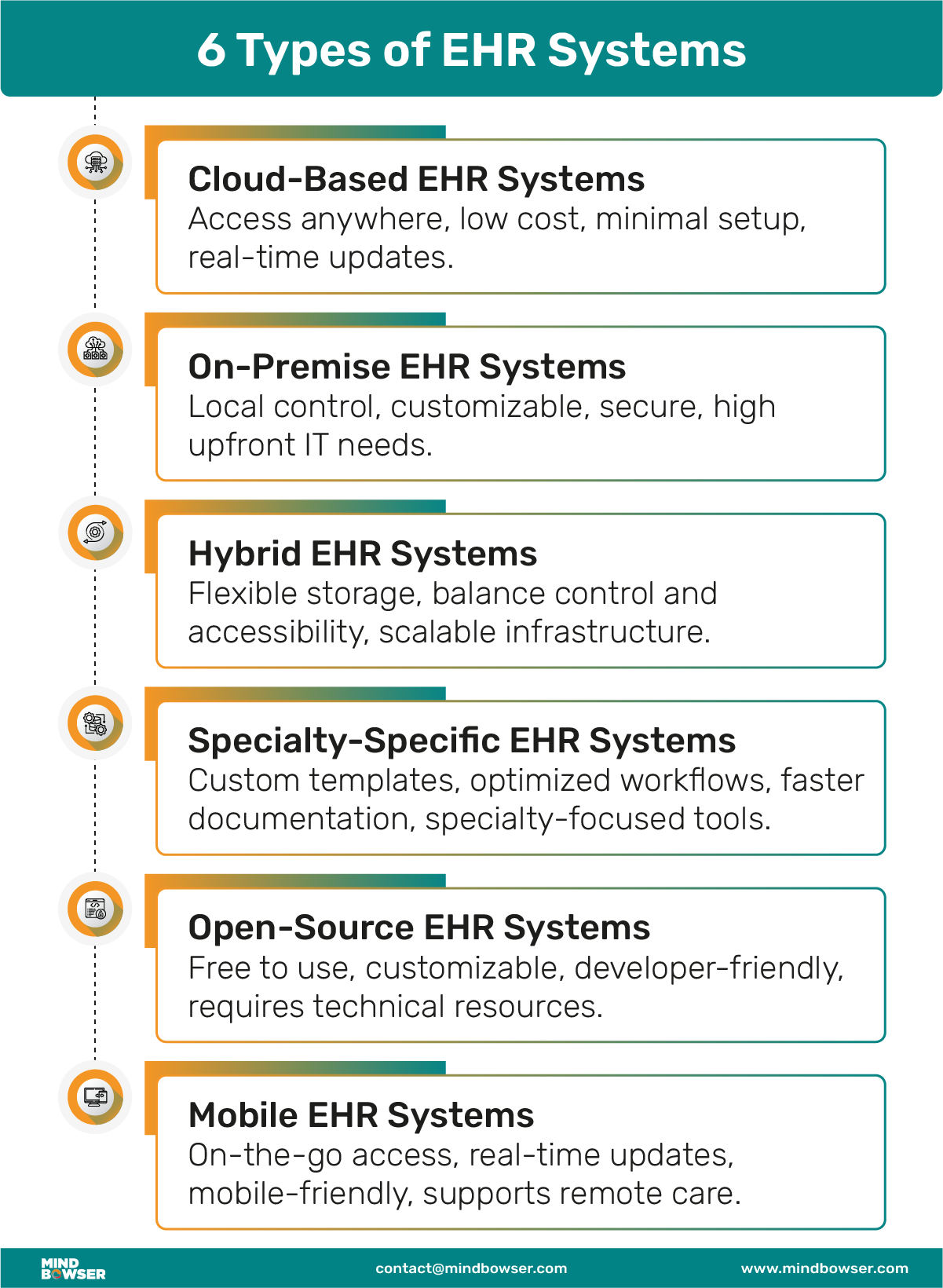
Specialty-specific EHR systems are designed for the unique needs of individual medical fields. Instead of a one-size-fits-all solution, these systems have features, templates, and workflows tailored to specialties like cardiology, orthopedics, dermatology, mental health, or pediatrics.
Imagine using a kitchen tool just for slicing sushi—it’s much more effective than a general-purpose knife. That’s what specialty-specific EHRs do for healthcare professionals.
A specialty-specific EHR system includes customized interfaces and modules based on how a particular specialty works. For example:
🔸 A dermatologist might need tools for high-resolution image capture and lesion tracking.
🔸 A psychiatrist may need detailed behavioral health notes, mood charts, and therapy session logs.
🔸 An orthopedic surgeon might prefer visual tools for joint mobility and surgical planning.
These systems eliminate unnecessary features and focus only on what matters to that practice.
These systems are especially helpful for:
🔸 Private practices with a single specialty
🔸 Clinics that want to avoid complex, generic EHRs
🔸 Specialists who need highly specific data capture and reporting tools
🔸 Faster documentation: Specialty templates reduce manual entry and speed up charting.
🔸 Improved accuracy: Built-in features align with specialty-specific workflows, reducing errors.
🔸 Better patient outcomes: Focused tools lead to more efficient diagnosis and treatment.
🔸 Higher user satisfaction: Physicians don’t need to wade through irrelevant options.
🔸 Limited scalability: May not work well if your clinic expands to multi-specialty services.
🔸 Vendor dependency: Fewer vendors specialize in niche EHRs, which could limit choices.
🔸 Integration concerns: Specialty EHRs might not integrate easily with hospital systems or lab interfaces.
Like other EHRs, specialty-specific systems must meet HIPAA and other healthcare data privacy standards. When choosing a system, ensure:
🔸 It supports secure messaging and access control.
🔸 Data export and interoperability options are available (e.g., HL7, FHIR compatibility).
A behavioral health clinic serving multiple therapists might choose a specialty-specific EHR that includes session note templates, mood trackers, patient self-assessments, and mental health billing codes. This system streamlines both patient care and administrative work.
Related Read: EMR vs EHR: What’s the Difference?
Open-source EHR systems give healthcare organizations full access to the software’s source code. This means the system can be customized and modified to fit specific needs—no vendor lock-in, no extra pay for changes.
It’s like building your own house from a blueprint you can edit, rather than renting one you can’t change.
An open-source EHR is software whose original code is made publicly available. Any healthcare provider, IT team, or third-party developer can:
🔸 Download the code
🔸 Modify it
🔸 Add features
🔸 Fix bugs
🔸 Create their version of the system
Popular examples include OpenMRS, GNU Health, and OpenEMR.
These systems are often used by:
🔸 Public health programs in developing countries
🔸 Academic institutions and research hospitals
🔸 Clinics with strong in-house tech teams
🔸 Startups looking for affordable, flexible EHR options
🔸 No licensing fees: Download and use it for free.
🔸 Full control: Customize features, workflows, and interfaces.
🔸 Community-driven innovation: Open-source projects often improve quickly thanks to developer contributions.
🔸 Interoperability potential: Easier to build in HL7, FHIR, or other healthcare data standards.
🔸 Technical expertise needed: Setup, customization, and updates require IT skills.
🔸 Lack of vendor support: You may not get professional customer service or documentation.
🔸 Security responsibility: You’re responsible for applying updates, patches, and securing patient data.
Related Read: Different Permissions and Possibilities Between Epic, Cerner, Athenahealth, and Meditech
Open-source doesn’t mean insecure. Many open-source EHRs follow strict HIPAA compliance protocols. But YOU must ensure:
🔸 Role-based access is set up
🔸 Data is encrypted
🔸 Backup systems are in place
🔸 Updates are applied regularly
A non-profit health organization operating clinics across multiple countries could use an open-source EHR like OpenMRS. With their tech team, they can customize the system in different languages, integrate with mobile devices, and ensure offline access in areas with poor internet connectivity.
Mobile EHR systems are designed to work on smartphones, tablets, and other handheld devices. They let healthcare providers access and update patient records from anywhere—whether in a clinic, on a hospital round, or visiting a patient’s home.
Think of them as your medical office in your pocket.
A mobile EHR is a version of an EHR platform optimized for mobile devices. It includes most of the same features you’d find on a desktop version, but with a responsive design and touch-friendly interface for ease of use on smaller screens.
Mobile EHR apps allow clinicians to:
🔸 View patient charts
🔸 Check lab results
🔸 Schedule appointments
🔸 Send secure messages
🔸 Update clinical notes in real time
Some apps also work offline and sync data once internet access is restored.
🔸 Home health and hospice care providers
🔸 Doctors working across multiple clinics or hospitals
🔸 Emergency responders
🔸 Rural or field-based healthcare workers
🔸 Providers offering telehealth services
🔸 On-the-go access: View or edit patient records anytime, from anywhere.
🔸 Faster documentation: Update notes during or after a visit, reducing missed details.
🔸 Improved care coordination: Real-time updates keep the whole care team in sync.
🔸 Patient engagement: Some mobile EHRs allow patients to interact with their records or receive appointment reminders.
🔸 Screen size constraints: Complex tasks like charting long notes may be harder on small screens.
🔸 Data entry speed: Typing large volumes on a mobile device can be slower.
🔸 Dependence on the internet: Limited offline functionality in some apps.
🔸 Device compatibility: Not all EHRs offer full-featured mobile versions.
Given the risk of data breaches from lost or stolen devices, mobile EHR systems include strong safeguards:
🔸 Password/PIN or biometric login (face/fingerprint recognition)
🔸 Automatic log-out after inactivity
🔸 Encrypted data transfer
🔸 Remote wipe capabilities for lost devices
HIPAA-compliant mobile EHRs are a must to ensure patient data privacy.
A visiting nurse providing home care can use a mobile EHR on a tablet to review a patient’s health history, document vitals, and update medication records—all in real time during the visit. This cuts down paperwork and improves record accuracy.
Related Read: The Impact of AI on Electronic Health Records
Choosing the right EHR system isn’t just a tech decision—it directly affects how smoothly your practice runs and how well you care for patients. With so many types of EHR systems available, aligning the choice with your organization’s size, specialty, workflow, and long-term goals is essential.
Here’s a simple breakdown to help you evaluate your options.
🔸 Small practices often benefit from cloud-based EHRs due to lower costs and a more straightforward setup.
🔸 Mid-sized and large organizations may prefer hybrid or on-premise systems for more control and customization.
🔸 If you operate in a niche field like dermatology, psychiatry, or orthopedics, a specialty-specific EHR will include the templates, forms, and workflows you need, without the clutter of irrelevant features.
🔸 If your staff provides home visits, telehealth, or field-based care, a mobile EHR with offline capabilities can boost efficiency and reduce paperwork.
🔸 Cloud-based and open-source systems are typically more affordable upfront.
🔸 On-premise systems come with high initial costs but may save money in the long term for large operations.
🔸 A cloud-based system with vendor-managed updates and support is ideal if your practice has little or no IT support.
🔸 Tech-savvy teams may prefer open-source or hybrid systems for full control and customization.
🔸 All systems should be HIPAA-compliant, but the level of responsibility varies:
🔹 Cloud providers handle most security protocols.
🔹 On-premise and open-source systems require in-house teams to manage encryption, backups, and access controls.
✅ Does it match your practice size and workflow?
✅ Is it easy to train staff on?
✅ Can it integrate with your labs, pharmacies, or billing tools?
✅ Is support available when you need it?
✅ Are updates automatic or manual?
✅ How easily can it scale as your practice grows?
Pro Tip – Before making a final decision, ask for a live demo or free trial. Let different team members, from doctors to front-desk staff, try the system. Real-world testing will reveal whether the system is intuitive and effective for your day-to-day operations.
If you want experienced EHR system providers who can help you align with your goals Mindbowser can help you. Let’s learn more:

At Mindbowser, we work with healthcare organizations at every stage of digital transformation, especially when it comes to building and integrating the right type of EHR system for their needs.
Whether you’re evaluating cloud-based, on-premise, hybrid, or specialty-specific solutions, we bring the experience, tools, and healthcare knowledge needed to move from decision to deployment without disruption.
We don’t offer off-the-shelf software. Instead, we work with you to build a custom EHR system that aligns with your workflows, specialty, and infrastructure. From specialty-specific templates to real-time documentation and HIPAA-compliant data storage, our solutions are built for scale and usability.
Using our HealthConnect CoPilot, we make it easy to integrate your EHR system with:
🔸 Major EHR platforms like Epic, Cerner, and Athenahealth
🔸 Health data standards including HL7, CCDA, and FHIR
🔸 Remote monitoring tools like Dexcom API, Apple Health API, and Fitbit API
This means better patient tracking, automated data sync, and interoperability out of the box.
We prioritize HIPAA, SOC 2, and GDPR compliance at every level—whether you choose a cloud-based, on-premise, or hybrid setup. We ensure:
🔸 Secure user authentication
🔸 Role-based access control
🔸 Encrypted storage and transmission
🔸 Audit logs and backup systems
Whether you’re leaning toward:
🔸 A cloud-based system for affordability and flexibility
🔸 An on-premise system for control and customization
🔸 A hybrid model for flexibility with redundancy
🔸 A mobile EHR for care on the move
🔸 A Specialty-specific EHR for your focused practice
—Mindbowser brings the experience and tools to deliver it.
We also help you scale, whether adding a telehealth module, integrating with third-party labs and pharmacies, or expanding across locations. Our modular architecture ensures that your EHR system grows with your organization.
Want to build or upgrade your EHR system the smart way?
Ready to streamline your healthcare operations with the perfect EHR? Contact our team for a personalized demo and start your journey to better patient care.
Cloud-based EHR systems are currently the most common due to their flexibility, cost-efficiency, and low maintenance.
Yes, but it’s usually more expensive and requires technical staff to manage. Cloud-based options are more budget-friendly for small practices.
Yes—if implemented correctly. You must ensure encryption, access control, and regular updates are in place.
Many modern specialty EHRs do. Be sure to check telehealth features like video calls, scheduling, and secure messaging.
Some mobile EHRs support offline access and sync once you’re back online. Always confirm this with your vendor.

We worked with Mindbowser on a design sprint, and their team did an awesome job. They really helped us shape the look and feel of our web app and gave us a clean, thoughtful design that our build team could...


The team at Mindbowser was highly professional, patient, and collaborative throughout our engagement. They struck the right balance between offering guidance and taking direction, which made the development process smooth. Although our project wasn’t related to healthcare, we clearly benefited...

Founder, Texas Ranch Security

Mindbowser played a crucial role in helping us bring everything together into a unified, cohesive product. Their commitment to industry-standard coding practices made an enormous difference, allowing developers to seamlessly transition in and out of the project without any confusion....

CEO, MarketsAI

I'm thrilled to be partnering with Mindbowser on our journey with TravelRite. The collaboration has been exceptional, and I’m truly grateful for the dedication and expertise the team has brought to the development process. Their commitment to our mission is...

Founder & CEO, TravelRite

The Mindbowser team's professionalism consistently impressed me. Their commitment to quality shone through in every aspect of the project. They truly went the extra mile, ensuring they understood our needs perfectly and were always willing to invest the time to...

CTO, New Day Therapeutics

I collaborated with Mindbowser for several years on a complex SaaS platform project. They took over a partially completed project and successfully transformed it into a fully functional and robust platform. Throughout the entire process, the quality of their work...

President, E.B. Carlson

Mindbowser and team are professional, talented and very responsive. They got us through a challenging situation with our IOT product successfully. They will be our go to dev team going forward.

Founder, Cascada

Amazing team to work with. Very responsive and very skilled in both front and backend engineering. Looking forward to our next project together.
Co-Founder, Emerge

The team is great to work with. Very professional, on task, and efficient.

Founder, PeriopMD

I can not express enough how pleased we are with the whole team. From the first call and meeting, they took our vision and ran with it. Communication was easy and everyone was flexible to our schedule. I’m excited to...

Founder, Seeke

We had very close go live timeline and Mindbowser team got us live a month before.

CEO, BuyNow WorldWide

Mindbowser brought in a team of skilled developers who were easy to work with and deeply committed to the project. If you're looking for reliable, high-quality development support, I’d absolutely recommend them.

Founder, Teach Reach

Mindbowser built both iOS and Android apps for Mindworks, that have stood the test of time. 5 years later they still function quite beautifully. Their team always met their objectives and I'm very happy with the end result. Thank you!

Founder, Mindworks

Mindbowser has delivered a much better quality product than our previous tech vendors. Our product is stable and passed Well Architected Framework Review from AWS.

CEO, PurpleAnt

I am happy to share that we got USD 10k in cloud credits courtesy of our friends at Mindbowser. Thank you Pravin and Ayush, this means a lot to us.

CTO, Shortlist

Mindbowser is one of the reasons that our app is successful. These guys have been a great team.

Founder & CEO, MangoMirror

Kudos for all your hard work and diligence on the Telehealth platform project. You made it possible.

CEO, ThriveHealth

Mindbowser helped us build an awesome iOS app to bring balance to people’s lives.

CEO, SMILINGMIND

They were a very responsive team! Extremely easy to communicate and work with!

Founder & CEO, TotTech

We’ve had very little-to-no hiccups at all—it’s been a really pleasurable experience.

Co-Founder, TEAM8s

Mindbowser was very helpful with explaining the development process and started quickly on the project.

Executive Director of Product Development, Innovation Lab

The greatest benefit we got from Mindbowser is the expertise. Their team has developed apps in all different industries with all types of social proofs.
Co-Founder, Vesica

Mindbowser is professional, efficient and thorough.

Consultant, XPRIZE

Very committed, they create beautiful apps and are very benevolent. They have brilliant Ideas.

Founder, S.T.A.R.S of Wellness

Mindbowser was great; they listened to us a lot and helped us hone in on the actual idea of the app. They had put together fantastic wireframes for us.

Co-Founder, Flat Earth

Mindbowser was incredibly responsive and understood exactly what I needed. They matched me with the perfect team member who not only grasped my vision but executed it flawlessly. The entire experience felt collaborative, efficient, and truly aligned with my goals.

Founder, Child Life On Call

The team from Mindbowser stayed on task, asked the right questions, and completed the required tasks in a timely fashion! Strong work team!

CEO, SDOH2Health LLC

Mindbowser was easy to work with and hit the ground running, immediately feeling like part of our team.

CEO, Stealth Startup

Mindbowser was an excellent partner in developing my fitness app. They were patient, attentive, & understood my business needs. The end product exceeded my expectations. Thrilled to share it globally.

Owner, Phalanx

Mindbowser's expertise in tech, process & mobile development made them our choice for our app. The team was dedicated to the process & delivered high-quality features on time. They also gave valuable industry advice. Highly recommend them for app development...

Co-Founder, Fox&Fork
