For many healthcare providers and transportation operators, relying on third-party NEMT vendors has become a double-edged sword. These platforms may offer quick onboarding, but they lock organizations into rigid workflows, escalate per-trip fees, and slow down product updates. The result is lost revenue, compliance risks, and limited control over patient experience.
By contrast, building a custom NEMT platform or investing in in-house NEMT software development enables organizations to control dispatch, billing, and compliance from end to end. Providers that replace third-party NEMT vendors with their own in-house dispatch system and NEMT billing software gain flexibility, ensure Medicaid-specific checks, and strengthen margins.
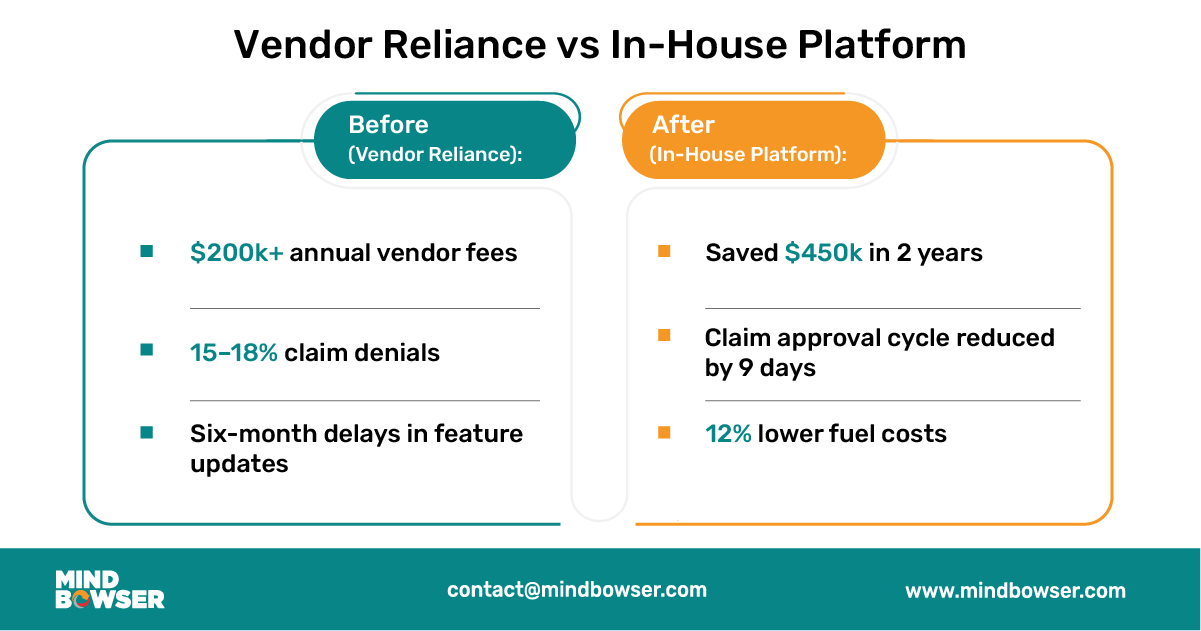
In short:
For years, many NEMT providers and healthcare organizations have turned to third-party platforms to simplify their operations. On the surface, these platforms appear to offer convenience. They offer ready-made dispatch systems, pre-configured billing modules, and standard compliance features. Yet behind this convenience lies a costly dependency that often undermines long-term sustainability.
Third-party vendors typically charge subscription fees that may appear affordable at first, but these fees quickly escalate as the fleet size and ride volume increase. A mid-sized provider with a fleet of 50 vehicles can pay tens of thousands of dollars annually in licensing and per-trip fees. This is money that could otherwise be invested in growing the fleet, training drivers, or upgrading compliance safeguards. Over time, these recurring expenses erode margins and make it harder for providers to compete in contracts that already operate on thin reimbursements.
Healthcare regulations evolve quickly. State Medicaid agencies often revise prior authorization rules, electronic visit verification requirements, or claim submission formats. When providers rely on an external vendor, they are at the mercy of that vendor’s product roadmap. Feature updates may take months or even years to materialize. In the meantime, providers are left with costly manual workarounds that increase denial rates and put compliance at risk.
For example, a provider in the Midwest shared how their vendor took almost a year to build an integration with a state Medicaid portal. During this period, the provider had to manually enter data into two systems, resulting in staff burnout, delayed reimbursements, and significant revenue loss.
Third-party systems are often designed for broad use, rather than being tailored to Medicaid rules or hospital workflows. This lack of customization makes integration with electronic medical records (EMRs) or Medicaid APIs challenging. Without seamless interoperability, providers face duplication of data entry, slower billing cycles, and a higher likelihood of errors that result in claim rejections.
Hospitals and payers increasingly expect transportation data to align with clinical workflows. If your NEMT software cannot integrate directly with EMRs, you are at a disadvantage when competing for contracts with health systems that prioritize data transparency and care coordination.
Perhaps the most frustrating challenge of relying on third parties is vendor lock-in. Providers that use a vendor’s platform rarely own the underlying code or data models. If they choose to switch vendors, migrating data becomes a complex and expensive process. Some vendors even impose fees or restrictions on data export, effectively trapping providers in an ecosystem that no longer serves their needs.
This creates a risky dependency. When the vendor changes pricing, sunsets features, or fails to meet compliance obligations, providers have little leverage to push back against these changes. The result is an environment where the vendor controls the pace of innovation and the provider absorbs the financial and operational consequences.
Building an in-house NEMT platform is not simply about replicating what a vendor offers. It is about creating a system that reflects the unique workflows of your organization, addresses compliance obligations, and ensures seamless integration across the healthcare ecosystem. A well-architected platform should cover every stage of the trip lifecycle, from scheduling and dispatch to billing and reporting. Below are the essential components that every provider should include when designing their own system.
Dispatching is the heartbeat of NEMT operations. Without precision and efficiency, providers face delays, patient dissatisfaction, and higher costs. An in-house dispatch module should include:
Providers that own their dispatch logic can continuously refine it, unlike vendors whose updates are delayed by broader customer backlogs.
Billing is where revenue is either secured or lost. An in-house billing system must be designed with Medicaid-specific requirements in mind, including:
By owning billing software, providers can align rules to their state’s Medicaid requirements instead of waiting for a vendor patch.
Compliance is non-negotiable in healthcare transportation. An in-house NEMT platform must embed compliance by design rather than treating it as an afterthought. Key features include:
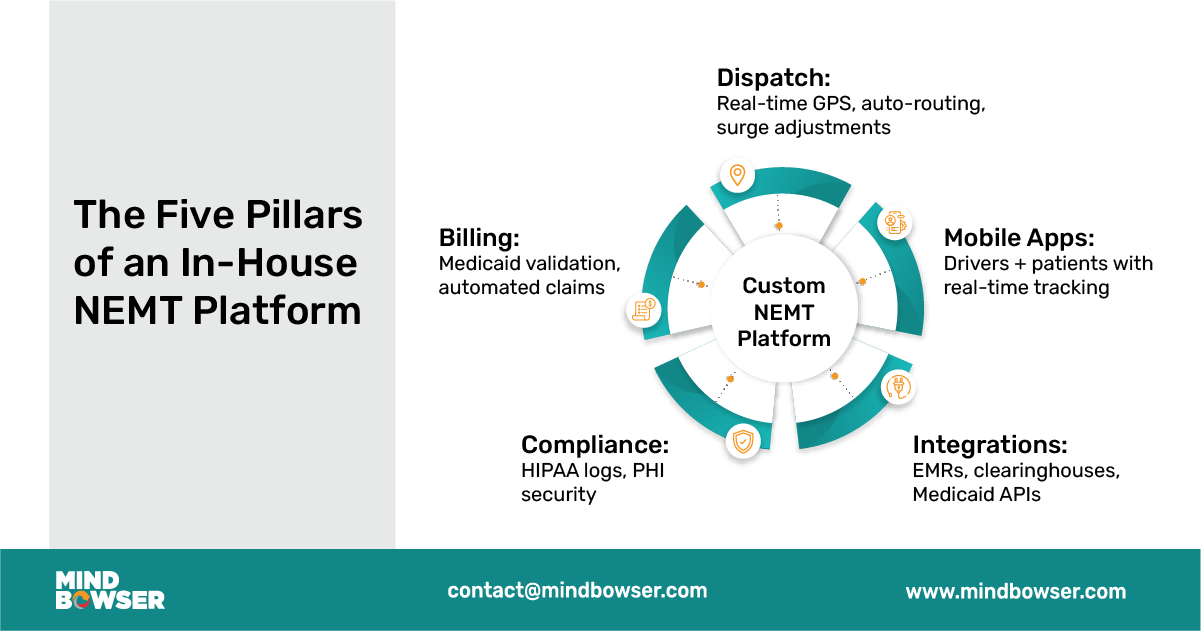
Transportation does not exist in isolation. Hospitals, payers, and brokers all expect integration. An in-house platform should be designed with interoperability at its core:
With ownership of the integration layer, providers can respond faster to evolving payer requirements and partnership opportunities.
The user experience matters just as much as back-office workflows. A comprehensive platform should include mobile applications tailored for both drivers and patients.
✅ Consultant’s Insight: The most successful in-house NEMT platforms are built around these five pillars. Dispatch and billing protect financial sustainability, compliance ensures long-term security, integrations enable partnerships, and mobile apps elevate patient experience. Together, they form a technology foundation that grows with the provider’s needs, rather than locking them into someone else’s roadmap.
it’s a systemic challenge across NEMT. The good news? Modern technology can stop the leaks before they drain your business. See how Mindbowser helps providers recover revenue and rebuild trust.
Shifting from a third-party NEMT vendor to a fully owned in-house system is a strategic transformation. It requires careful planning, stakeholder buy-in, and phased execution. The good news is that the process can be structured to minimize disruption and deliver measurable results at each stage. Below is a proven roadmap that organizations can follow to replace external platforms with a custom-built NEMT solution.
The first step is to understand exactly how your organization operates today. Many providers underestimate the hidden inefficiencies in their processes until they are documented.
Deliverable: A detailed requirements document that highlights what your in-house NEMT dispatch system and billing platform must achieve.
Once the requirements are clear, the next step is to translate them into early prototypes.
This phase ensures that the platform accurately reflects actual workflows rather than assumptions made by leadership or developers.
The foundation of any NEMT system lies in dispatch and billing. These two modules have a direct impact on revenue, compliance, and patient satisfaction.
Focusing on these areas first delivers quick wins and builds staff confidence.
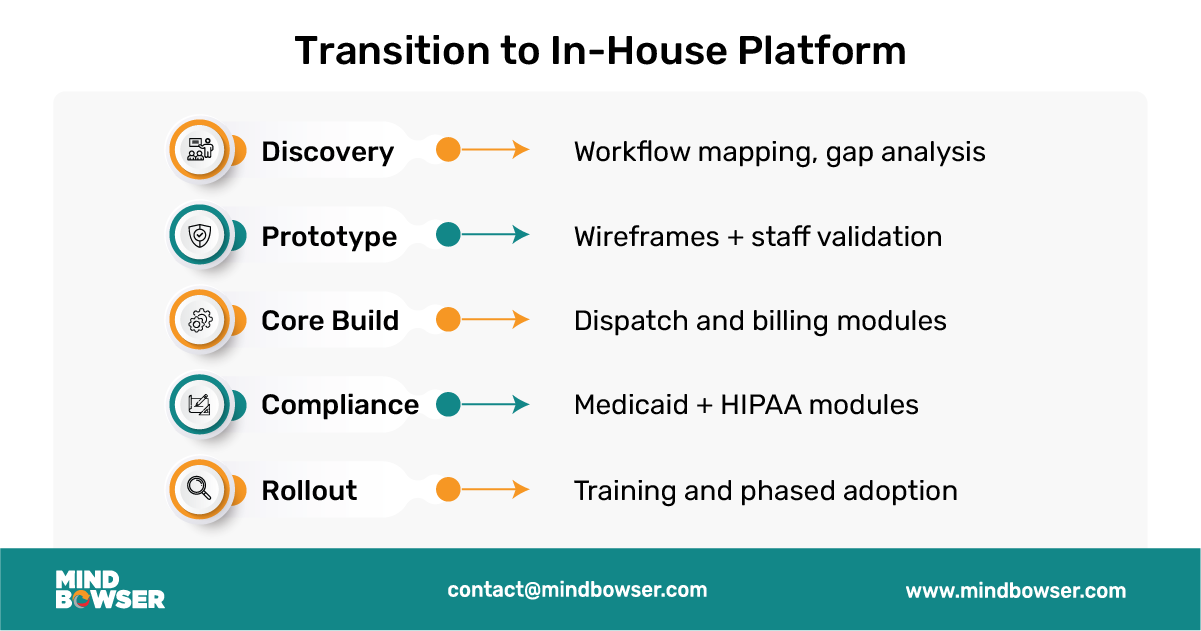
With dispatch and billing operational, the next priority is compliance and integration.
This phase transforms the system from a scheduling tool into a compliance-ready healthcare platform.
Technology adoption succeeds only when people are prepared to use it. A phased rollout avoids overwhelming staff and allows for smooth adjustments.
Deliverable: A fully operational in-house NEMT platform that mirrors your workflows and scales to future needs.
✅ Consultant’s Insight: The transition to an in-house platform is not an overnight project. By breaking it into structured steps, providers minimize risk while building long-term capacity. The focus should always be on aligning technology with workflows, rather than forcing staff to use rigid, vendor-designed systems.
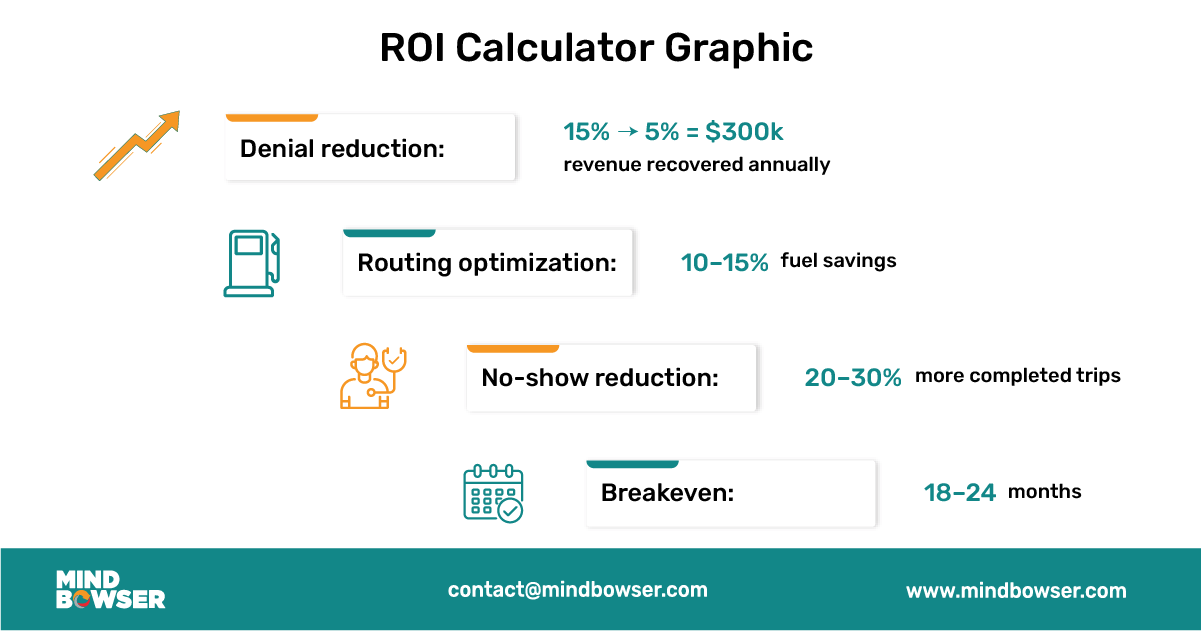
Every NEMT provider knows that margins are thin, and financial decisions must be backed by measurable return on investment. The decision to build a custom in-house NEMT platform often raises questions about cost and payback. While there is an upfront investment, the long-term economics and strategic benefits consistently favor ownership. By comparing the total cost of ownership, understanding breakeven timelines, and factoring in the hidden value of intellectual property, providers can make a confident business case.
Third-party NEMT vendors typically operate on a subscription model with licensing and per-trip fees. At first glance, this seems manageable. However, over the course of three years, these recurring costs far exceed the upfront investment in a custom platform.
In short, what appears “cheaper” in the beginning becomes more expensive over time when relying on third-party vendors.
For most providers, the breakeven point for an in-house platform occurs within 18 to 24 months. The reason is that the system not only reduces vendor fees but also recovers revenue that is commonly lost under third-party solutions.
When these savings are combined, the upfront investment pays for itself quickly and every year thereafter represents pure financial benefit.
Return on investment is not only financial; it also encompasses non-financial benefits. Owning a custom-built NEMT platform also creates strategic value.
While the ROI numbers are compelling, the most important benefit of building in-house is strategic control. Providers no longer worry about sudden vendor price increases, delayed compliance updates, or the risk of data lock-in. Instead, they decide the pace of innovation, the scope of compliance, and the roadmap for patient experience improvements.
✅ Consultant’s Insight: The upfront investment in building a custom NEMT platform is best understood as an asset, not an expense. Within two years, most providers achieve breakeven, and within five years, they often enjoy returns exceeding 300 percent. More importantly, they gain independence, compliance agility, and the ability to grow on their own terms.
Even when the advantages of an in-house NEMT platform are clear, many providers hesitate to leap. The hesitation is understandable. Healthcare organizations already operate under tight budgets, heavy compliance requirements, and thin staffing. Building a custom dispatch and billing platform feels like a daunting project. However, most of the fears that surface during the decision process can be anticipated and addressed with a structured approach.
Many NEMT operators lack large technology teams. Dispatchers and billing staff are comfortable with existing tools, and leadership worries that building a custom platform will overwhelm them.
How to Overcome:
Cost overruns are a common concern with custom software projects. Providers fear starting with one budget and ending up with double the expense.
How to Overcome:
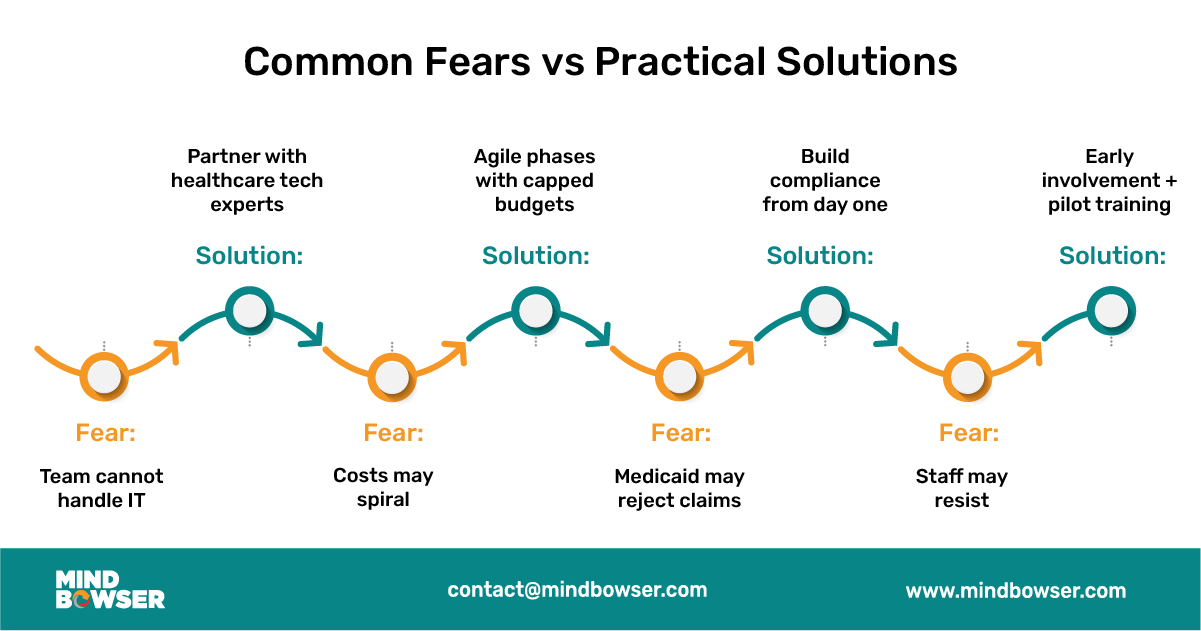
Providers often worry that Medicaid will reject claims submitted through a custom-built platform, leaving them with compliance and reimbursement risks.
How to Overcome:
Change management is often overlooked. Even the best technology can fail if staff are reluctant to adopt it.
How to Overcome:
Sometimes the best way to understand the value of moving away from third-party vendors is to see what happens when a provider leaps. The following real-world case illustrates how a mid-sized operator transformed its operations, finances, and compliance posture by building its own NEMT platform.
The provider, based in New York, managed a fleet of 60 vehicles and served several counties under Medicaid contracts. For years, they relied on a well-known third-party NEMT vendor to handle dispatch and billing. Initially, the platform appeared sufficient. Over time, however, the cracks began to show:
The leadership team realized that as long as they remained tied to a third-party vendor, they would be reactive rather than proactive in a highly competitive market.
In 2021, the provider decided to build its own in-house NEMT dispatch and billing system. They partnered with a healthcare-focused technology firm and followed a phased implementation plan:
The results were significant and measurable within two years:
For many providers, the choice between off-the-shelf vendor solutions and a custom in-house build feels like a trade-off between convenience and complexity. Off-the-shelf platforms promise quick deployment and lower upfront costs, but they come with long-term limitations. In contrast, custom platforms require a deliberate investment but provide unmatched control, scalability, and ownership. When evaluated over the long horizon, custom platforms consistently prove to be the superior choice.
Off-the-shelf platforms are designed to cater to the average provider, rather than the unique needs of each organization. As a result, when Medicaid rules change or new features are needed, providers are forced to wait on the vendor’s roadmap. This can result in months of delays while compliance gaps widen and revenue leaks increase.
A custom-built system avoids this trap. Because the provider owns the code, updates can be implemented immediately. Whether it is adding a new Medicaid billing rule, adjusting audit logs, or integrating with a hospital’s electronic health record, changes happen on the provider’s schedule rather than the vendor’s.
One of the most overlooked costs in third-party systems is the per-trip fee structure. For providers handling thousands of trips per month, these fees add up quickly and drain margins. Over the course of several years, per-trip fees often exceed the cost of building an in-house dispatch system entirely.
A custom platform eliminates these recurring charges. The more trips a provider delivers, the more cost-efficient the system becomes. This creates scalability that grows with the business, rather than punishing it for success.
Healthcare transportation is evolving rapidly. What works today may not meet requirements in three years. Off-the-shelf systems are rigid and offer limited flexibility for adding new features, such as artificial intelligence, predictive scheduling, or expanded integrations with payers.
With a custom platform, scalability is unlimited. Providers can begin with core dispatch and billing functions, then gradually add advanced analytics, clearinghouse integrations, or ride-share partnerships. This modular approach ensures that the platform grows in tandem with the organization, making it a long-term asset rather than a temporary solution.
While off-the-shelf systems appear less expensive initially, the cumulative cost of subscriptions, per-trip fees, and missed revenue from claim denials far outweighs the upfront expense of building in-house. By the third or fourth year, most providers realize that their custom platform is not only more cost-effective but also more profitable, as it protects revenue streams that vendors cannot.
Owning the platform means owning the data and the rules that govern it. With vendor systems, data is often siloed, difficult to export, or tied up in proprietary formats. This creates risk when negotiating with payers, preparing for audits, or considering mergers and acquisitions.
A custom system places full control in the provider’s hands. Intellectual property ownership also opens doors to future revenue opportunities. A provider could license modules to smaller operators, resell the technology, or leverage the platform to negotiate stronger contracts with Medicaid and hospital partners.

The Non-Emergency Medical Transportation sector is at a crossroads. For too long, providers have depended on third-party vendors that offer limited flexibility, recurring costs, and delayed innovation. While these platforms may have provided a stepping stone for digitization, they are no longer sufficient in an environment defined by strict Medicaid compliance, thin margins, and increasing demands for transparency.
Building an in-house NEMT platform changes the equation. Providers that make this move gain complete ownership of their dispatch systems, billing workflows, and compliance safeguards. They no longer wait for vendors to update features or struggle with locked data. Instead, they adapt in real time to state Medicaid rules, integrate directly with hospital systems, and create patient experiences that strengthen trust.
The business case is equally compelling. Within 18 to 24 months, most mid-sized providers achieve a break-even point on their investment. Beyond that point, they enjoy ongoing financial advantages, including elimination of per-trip fees, lower denial rates, and improved cash flow from faster reimbursements. Intellectual property ownership further strengthens valuations, attracts investors, and positions providers as long-term partners in healthcare ecosystems.
Perhaps most importantly, a custom-built NEMT platform empowers providers to control their own future. They decide when to incorporate artificial intelligence for predictive dispatching, when to expand into ride-sharing integrations, or when to enhance patient portals for improved engagement. Instead of being trapped in someone else’s roadmap, they own the path forward.
✅ Consultant’s Insight: In a fragmented market where compliance, efficiency, and patient satisfaction determine survival, technology ownership is no longer optional. Providers that build their own platforms take control of their margins, their contracts, and their destiny.
If your organization is still tied to a third-party vendor, now is the time to evaluate alternatives. Every month of delay means more revenue lost to fees, denials, and inefficiencies.
Thinking of breaking free from third-party vendors? Let us help you build your own dispatch and billing platform.
The future of NEMT belongs to providers who take ownership of their technology. The question is not whether you can afford to build in-house; rather, it is whether you can afford not to. The real question is how much longer you can afford not to.

We worked with Mindbowser on a design sprint, and their team did an awesome job. They really helped us shape the look and feel of our web app and gave us a clean, thoughtful design that our build team could...


The team at Mindbowser was highly professional, patient, and collaborative throughout our engagement. They struck the right balance between offering guidance and taking direction, which made the development process smooth. Although our project wasn’t related to healthcare, we clearly benefited...

Founder, Texas Ranch Security

Mindbowser played a crucial role in helping us bring everything together into a unified, cohesive product. Their commitment to industry-standard coding practices made an enormous difference, allowing developers to seamlessly transition in and out of the project without any confusion....

CEO, MarketsAI

I'm thrilled to be partnering with Mindbowser on our journey with TravelRite. The collaboration has been exceptional, and I’m truly grateful for the dedication and expertise the team has brought to the development process. Their commitment to our mission is...

Founder & CEO, TravelRite

The Mindbowser team's professionalism consistently impressed me. Their commitment to quality shone through in every aspect of the project. They truly went the extra mile, ensuring they understood our needs perfectly and were always willing to invest the time to...

CTO, New Day Therapeutics

I collaborated with Mindbowser for several years on a complex SaaS platform project. They took over a partially completed project and successfully transformed it into a fully functional and robust platform. Throughout the entire process, the quality of their work...

President, E.B. Carlson

Mindbowser and team are professional, talented and very responsive. They got us through a challenging situation with our IOT product successfully. They will be our go to dev team going forward.

Founder, Cascada

Amazing team to work with. Very responsive and very skilled in both front and backend engineering. Looking forward to our next project together.
Co-Founder, Emerge

The team is great to work with. Very professional, on task, and efficient.

Founder, PeriopMD

I can not express enough how pleased we are with the whole team. From the first call and meeting, they took our vision and ran with it. Communication was easy and everyone was flexible to our schedule. I’m excited to...

Founder, Seeke

We had very close go live timeline and Mindbowser team got us live a month before.

CEO, BuyNow WorldWide

Mindbowser brought in a team of skilled developers who were easy to work with and deeply committed to the project. If you're looking for reliable, high-quality development support, I’d absolutely recommend them.

Founder, Teach Reach

Mindbowser built both iOS and Android apps for Mindworks, that have stood the test of time. 5 years later they still function quite beautifully. Their team always met their objectives and I'm very happy with the end result. Thank you!

Founder, Mindworks

Mindbowser has delivered a much better quality product than our previous tech vendors. Our product is stable and passed Well Architected Framework Review from AWS.

CEO, PurpleAnt

I am happy to share that we got USD 10k in cloud credits courtesy of our friends at Mindbowser. Thank you Pravin and Ayush, this means a lot to us.

CTO, Shortlist

Mindbowser is one of the reasons that our app is successful. These guys have been a great team.

Founder & CEO, MangoMirror

Kudos for all your hard work and diligence on the Telehealth platform project. You made it possible.

CEO, ThriveHealth

Mindbowser helped us build an awesome iOS app to bring balance to people’s lives.

CEO, SMILINGMIND

They were a very responsive team! Extremely easy to communicate and work with!

Founder & CEO, TotTech

We’ve had very little-to-no hiccups at all—it’s been a really pleasurable experience.

Co-Founder, TEAM8s

Mindbowser was very helpful with explaining the development process and started quickly on the project.

Executive Director of Product Development, Innovation Lab

The greatest benefit we got from Mindbowser is the expertise. Their team has developed apps in all different industries with all types of social proofs.
Co-Founder, Vesica

Mindbowser is professional, efficient and thorough.

Consultant, XPRIZE

Very committed, they create beautiful apps and are very benevolent. They have brilliant Ideas.

Founder, S.T.A.R.S of Wellness

Mindbowser was great; they listened to us a lot and helped us hone in on the actual idea of the app. They had put together fantastic wireframes for us.

Co-Founder, Flat Earth

Mindbowser was incredibly responsive and understood exactly what I needed. They matched me with the perfect team member who not only grasped my vision but executed it flawlessly. The entire experience felt collaborative, efficient, and truly aligned with my goals.

Founder, Child Life On Call

The team from Mindbowser stayed on task, asked the right questions, and completed the required tasks in a timely fashion! Strong work team!

CEO, SDOH2Health LLC

Mindbowser was easy to work with and hit the ground running, immediately feeling like part of our team.

CEO, Stealth Startup

Mindbowser was an excellent partner in developing my fitness app. They were patient, attentive, & understood my business needs. The end product exceeded my expectations. Thrilled to share it globally.

Owner, Phalanx

Mindbowser's expertise in tech, process & mobile development made them our choice for our app. The team was dedicated to the process & delivered high-quality features on time. They also gave valuable industry advice. Highly recommend them for app development...

Co-Founder, Fox&Fork
