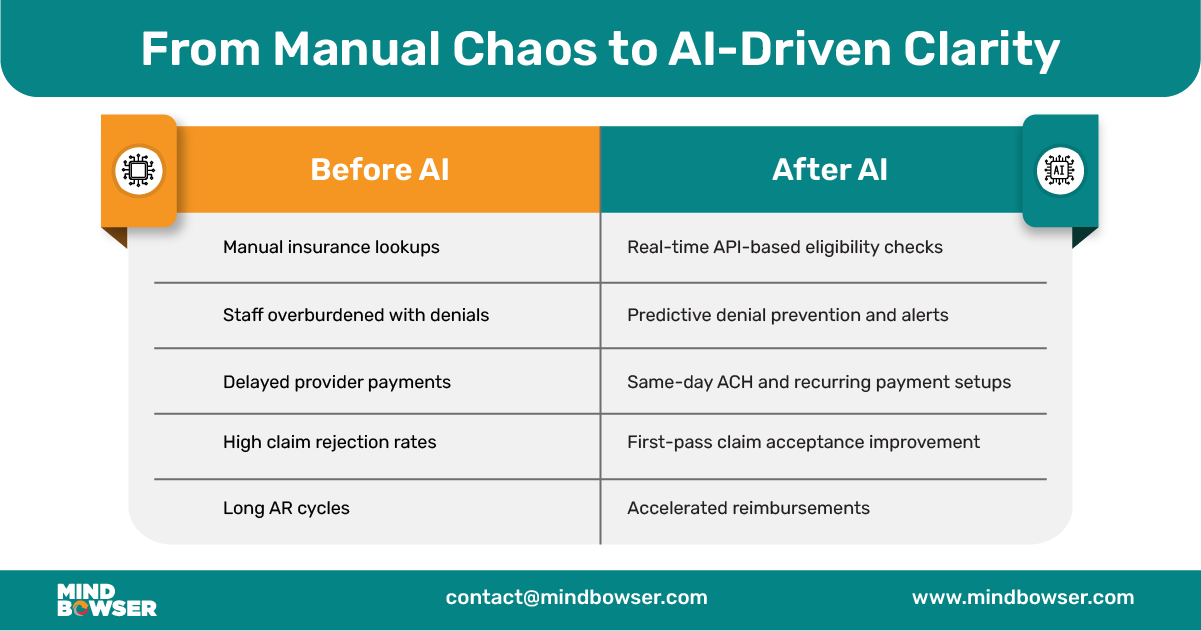
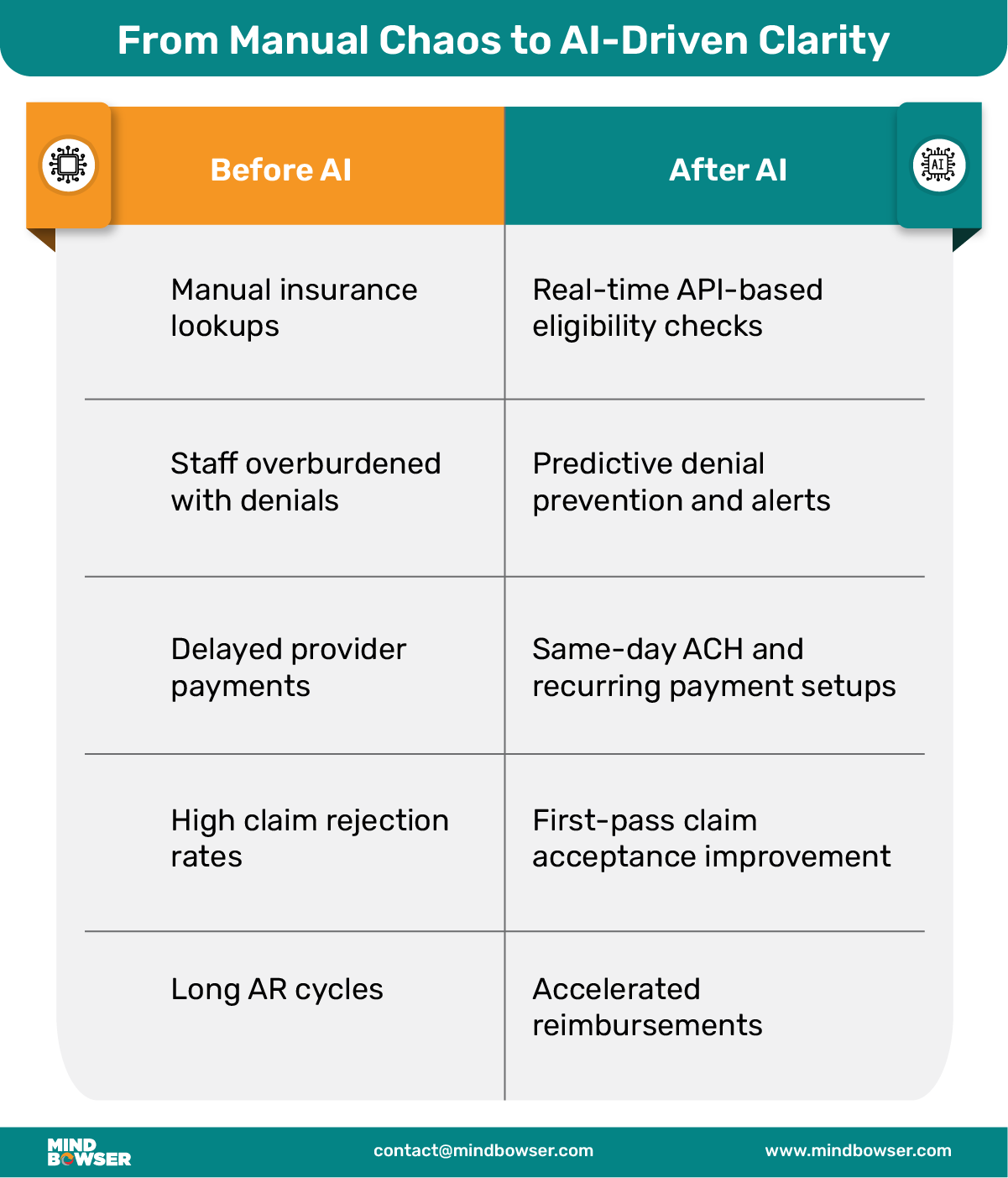
Healthcare revenue teams are being stretched thin. Every day brings new payer requirements, updated codes, and fewer hands to do the work. Manual processes—like checking insurance, entering codes, and resolving denials—slow things down and create room for mistakes. Over time, those small errors pile up into delayed payments and lost revenue.
AI isn’t a silver bullet, but it’s convenient when applied right. It takes on repetitive tasks that eat up staff time and cause burnout. It checks for gaps before claims go out, learns from denials, and keeps your payment workflows running without constant follow-ups. It’s not about replacing people—it’s about letting them focus on work that needs a human brain.
At Mindbowser, we bring AI into healthcare revenue cycle management with one goal: to make the system faster and smarter without breaking what already works. We can help you connect directly to your EHR, integrate with payer APIs, and stay HIPAA-compliant. Whether it’s automating eligibility checks or scrubbing claims before submission, we focus on what moves the needle.
Revenue Cycle Management (RCM) covers every step between when a patient schedules an appointment and when the provider gets paid. It sounds straightforward, but it’s anything but simple in practice.
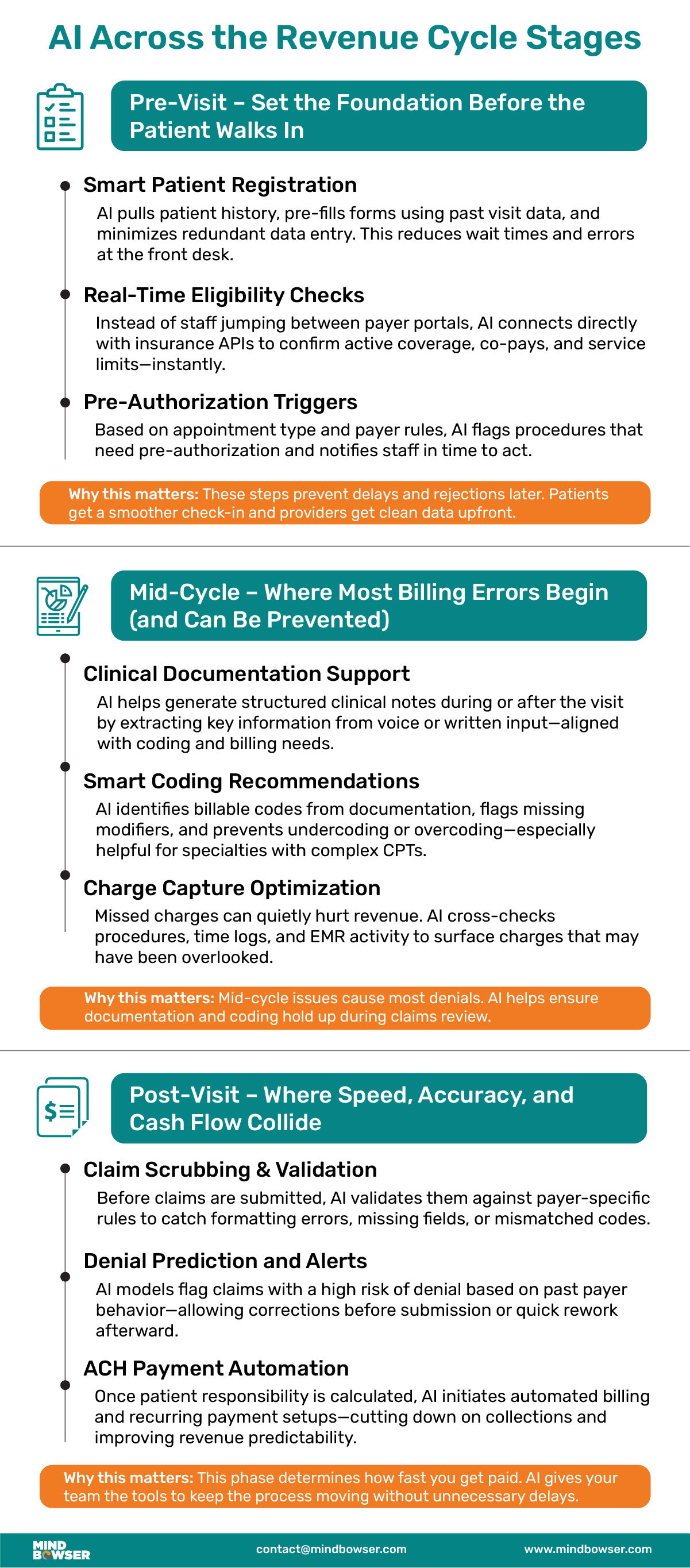
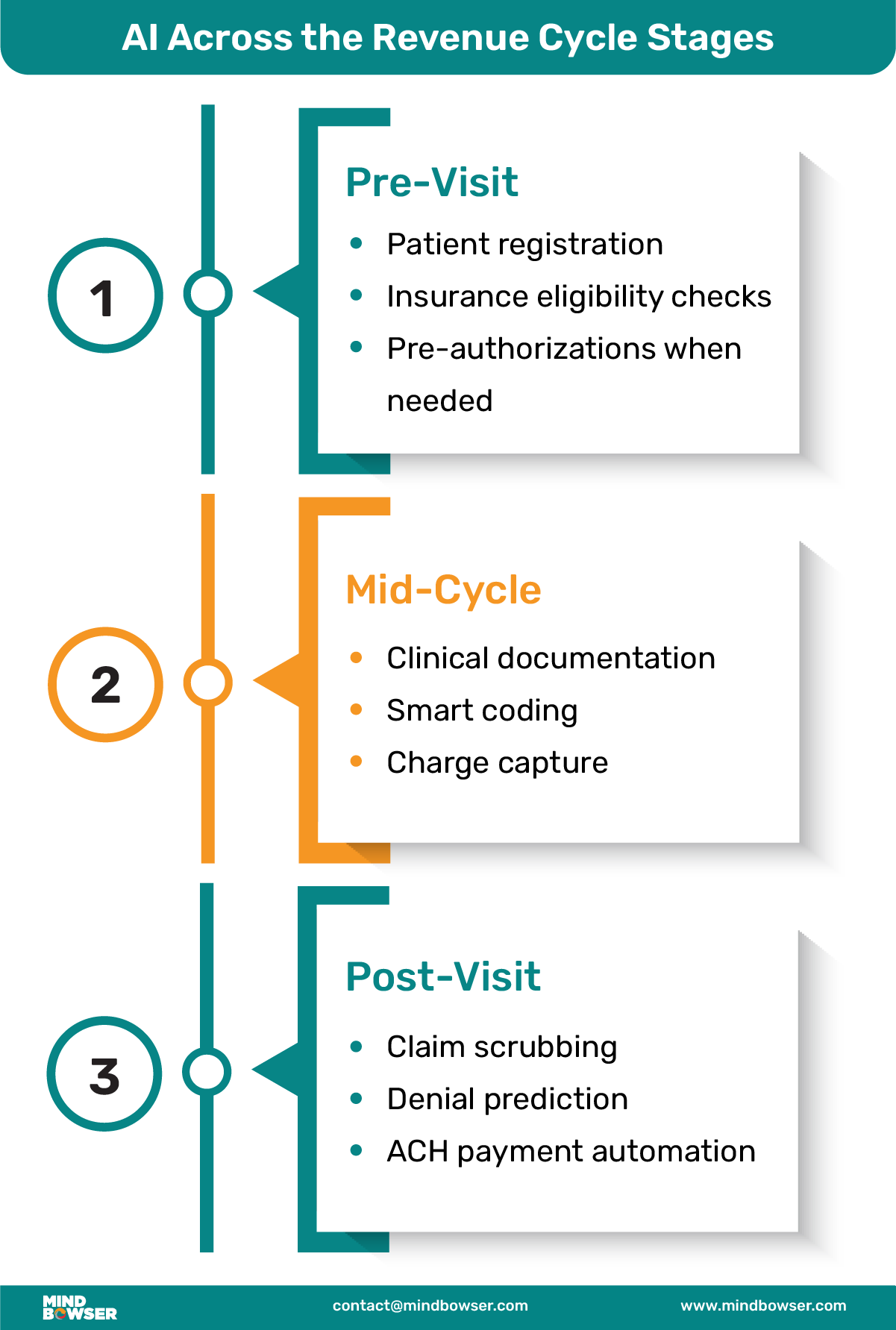
🔸 Pre-visit
This stage lays the groundwork for everything that follows. It includes:
🔸 Mid-cycle
Once care is delivered, the focus shifts to proper documentation and billing:
🔸 Post-visit
The financial work continues well after the appointment ends:
Most problems in RCM come down to timing and manual effort. Here’s what usually gets in the way:
The result? Providers wait longer to get paid, patients get frustrated, and teams lose time chasing paperwork instead of focusing on outcomes.
AI can add serious value without the need to rewire your entire system. When you apply it to key steps within the revenue cycle, it saves time, lowers error rates, and helps claims move faster—all without making things more complicated for your team.
One of the most time-consuming and error-prone tasks is verifying whether a patient’s insurance is active and what it covers. Every missed co-pay or overlooked deductible adds friction—not just for billing, but for patient trust too.
AI solves this by pulling real-time data directly from payer APIs and matching it with patient records. This means front-desk staff no longer need to toggle between portals or re-enter the same information in multiple places.
With our solution accelerators, this process now takes 15–20 minutes less per patient. It reduces redundancy and cuts down on human errors. More importantly, it gives your team confidence that every patient walking in has verified coverage, right from the start.
Medical coding mistakes are among the biggest causes of claim delays and denials. They also lead to underpayments or payer audits. The challenge is that coding requires accuracy, but most teams are juggling time pressure, complex rules, and ever-changing billing guidelines.
That’s where AI proves its worth. It can read clinical notes and suggest CPT or ICD codes based on what was actually documented. It doesn’t guess—it identifies patterns, flags inconsistencies, and ensures every claim is backed by supporting data.
We don’t offer a black box tool. We build coding assistants that plug directly into your current EHR setup, tailored to your specialty. Over time, they learn your most common diagnoses, procedures, and documentation habits—making the system more accurate the more you use it.
Related read: Medical Billing vs Revenue Cycle Management: What’s the Real Difference?
A clean claim is a paid claim. But even small issues—like missing modifiers or formatting errors—can get a claim denied on the first pass, starting a frustrating cycle of corrections and resubmissions.
AI-driven scrubbing tools go over each claim with a fine-toothed comb before it ever leaves your system. They validate fields, check against the specific payer’s rules, and catch anything that might trigger a rejection. They also adapt based on new rules as payers update them.
By fixing issues at the source, this step dramatically improves first-pass acceptance rates and shortens reimbursement cycles. It’s like giving your billing team a superpower—without adding more headcount.
Claim denials will always be a part of the game—but that doesn’t mean you can’t see them coming. AI analyzes your historical claim data to spot patterns that often lead to denials, like missing documentation or incorrect authorization.
More than just alerting your team to high-risk claims, our tools are built to learn over time. They adapt based on feedback, improving with each cycle. This means the system doesn’t just identify problems—it gets better at preventing them.
We’ve embedded this logic into our RCM tools, creating feedback loops that reduce repeated mistakes and accelerate resolution timelines. It’s denial management that works before the denial even happens.
Unpaid balances and billing confusion can kill cash flow—and hurt the patient experience. Many patients don’t know what they’ll owe until they get the bill weeks later. Providers, meanwhile, face collection challenges that eat into revenue.
AI fixes this by giving you accurate, upfront estimates of patient responsibility—based on real-time eligibility checks, service codes, and historical trends. This allows your team to collect at the point of service or set up payment plans early.
We applied this model for one of our clients by building a secure ACH-based payment system. It allowed them to process both one-time and recurring payments with ease. Patients could approve charges instantly or set up installment plans—all from their phones. Providers saw faster payments, reduced collection costs, and happier patients.
Related read: Future of Healthcare Revenue Cycle Management
You don’t need to reinvent your tech stack to benefit from AI. At Mindbowser, we focus on practical integration—plugging AI into your existing systems to deliver value fast, without disrupting your team’s daily routine.
We’ve built over 50 solution accelerators that serve as building blocks for common RCM challenges. That means:
Whether you use Epic EHR, Cerner EHR, or Athenahealth EHR, we make the connection work.
Security and compliance aren’t optional in healthcare. Every tool we build follows strict rules for data protection. That includes:
Your AI tools are only as good as the systems they talk to. We specialize in integrating with:
Whether it’s real-time eligibility, claims submission, or denial tracking, we make sure the data moves securely and accurately between all systems.
AI in revenue cycle management isn’t plug-and-play. When done thoughtfully, it delivers real results. However, the right approach can introduce more problems than it solves.
“Generative AI tools are powerful, but you need human oversight to prevent hallucinations and maintain safety in healthcare systems.”
— Mohan Giridharadas, LeanTaaS CEO
If AI tools are trained on incomplete or outdated billing data, they’ll make poor decisions, misidentifying codes, missing payer nuances, or flagging incorrect claims.
We focus on training models using your historical data and payer-specific rules to avoid blind spots from day one.
Introducing workflow automation without context can overwhelm your staff. If billing or front-desk teams don’t understand or trust the new system, adoption will stall.
We address this by starting small, running pilots, and offering team training to build buy-in as results become visible.
Connecting your EHR with payer systems, payment processors, and clearinghouses isn’t always straightforward. One poorly mapped field can break claims or lead to compliance gaps.
We avoid this by using structured data formats (like JSON), clear mapping documentation, and automated validation checkpoints at every handoff.
Automated systems can expose you to regulatory risks without proper tracking and role-based access, from HIPAA violations to audit failures.
Our tools are designed with built-in logging, secure access controls, and audit-ready trails, keeping every transaction transparent and compliant.
Assign a dedicated integration expert to manage system mapping and validation

If your revenue team is buried in claim edits, chasing denials, or losing hours to insurance lookups, it’s time to rework the system.
At Mindbowser, we don’t sell generic platforms. We work alongside your team to build what fits:
Whether managing a dental group, an outpatient clinic, or launching a new health plan, we help you integrate AI where it works best: inside your existing tech, with measurable results from week one.
Curious how an AI-driven RCM system can transform your operations? Discover how HealthConnect CoPilot seamlessly connects your systems—without the usual integration headaches. Get in touch with our team to see it in action.
If your team spends hours on manual eligibility, sees frequent claim denials, or uses disconnected tools—it’s a sign your RCM could benefit from automation.
Yes. With our integration layer (HealthConnect CoPilot), we support Epic, Cerner, Athenahealth, Open Dental, and more.
With our accelerators, most teams go live in weeks, not months—starting with pilot modules and expanding from there.

We worked with Mindbowser on a design sprint, and their team did an awesome job. They really helped us shape the look and feel of our web app and gave us a clean, thoughtful design that our build team could...


The team at Mindbowser was highly professional, patient, and collaborative throughout our engagement. They struck the right balance between offering guidance and taking direction, which made the development process smooth. Although our project wasn’t related to healthcare, we clearly benefited...

Founder, Texas Ranch Security

Mindbowser played a crucial role in helping us bring everything together into a unified, cohesive product. Their commitment to industry-standard coding practices made an enormous difference, allowing developers to seamlessly transition in and out of the project without any confusion....

CEO, MarketsAI

I'm thrilled to be partnering with Mindbowser on our journey with TravelRite. The collaboration has been exceptional, and I’m truly grateful for the dedication and expertise the team has brought to the development process. Their commitment to our mission is...

Founder & CEO, TravelRite

The Mindbowser team's professionalism consistently impressed me. Their commitment to quality shone through in every aspect of the project. They truly went the extra mile, ensuring they understood our needs perfectly and were always willing to invest the time to...

CTO, New Day Therapeutics

I collaborated with Mindbowser for several years on a complex SaaS platform project. They took over a partially completed project and successfully transformed it into a fully functional and robust platform. Throughout the entire process, the quality of their work...

President, E.B. Carlson

Mindbowser and team are professional, talented and very responsive. They got us through a challenging situation with our IOT product successfully. They will be our go to dev team going forward.

Founder, Cascada

Amazing team to work with. Very responsive and very skilled in both front and backend engineering. Looking forward to our next project together.
Co-Founder, Emerge

The team is great to work with. Very professional, on task, and efficient.

Founder, PeriopMD

I can not express enough how pleased we are with the whole team. From the first call and meeting, they took our vision and ran with it. Communication was easy and everyone was flexible to our schedule. I’m excited to...

Founder, Seeke

We had very close go live timeline and Mindbowser team got us live a month before.

CEO, BuyNow WorldWide

Mindbowser brought in a team of skilled developers who were easy to work with and deeply committed to the project. If you're looking for reliable, high-quality development support, I’d absolutely recommend them.

Founder, Teach Reach

Mindbowser built both iOS and Android apps for Mindworks, that have stood the test of time. 5 years later they still function quite beautifully. Their team always met their objectives and I'm very happy with the end result. Thank you!

Founder, Mindworks

Mindbowser has delivered a much better quality product than our previous tech vendors. Our product is stable and passed Well Architected Framework Review from AWS.

CEO, PurpleAnt

I am happy to share that we got USD 10k in cloud credits courtesy of our friends at Mindbowser. Thank you Pravin and Ayush, this means a lot to us.

CTO, Shortlist

Mindbowser is one of the reasons that our app is successful. These guys have been a great team.

Founder & CEO, MangoMirror

Kudos for all your hard work and diligence on the Telehealth platform project. You made it possible.

CEO, ThriveHealth

Mindbowser helped us build an awesome iOS app to bring balance to people’s lives.

CEO, SMILINGMIND

They were a very responsive team! Extremely easy to communicate and work with!

Founder & CEO, TotTech

We’ve had very little-to-no hiccups at all—it’s been a really pleasurable experience.

Co-Founder, TEAM8s

Mindbowser was very helpful with explaining the development process and started quickly on the project.

Executive Director of Product Development, Innovation Lab

The greatest benefit we got from Mindbowser is the expertise. Their team has developed apps in all different industries with all types of social proofs.
Co-Founder, Vesica

Mindbowser is professional, efficient and thorough.

Consultant, XPRIZE

Very committed, they create beautiful apps and are very benevolent. They have brilliant Ideas.

Founder, S.T.A.R.S of Wellness

Mindbowser was great; they listened to us a lot and helped us hone in on the actual idea of the app. They had put together fantastic wireframes for us.

Co-Founder, Flat Earth

Mindbowser was incredibly responsive and understood exactly what I needed. They matched me with the perfect team member who not only grasped my vision but executed it flawlessly. The entire experience felt collaborative, efficient, and truly aligned with my goals.

Founder, Child Life On Call

The team from Mindbowser stayed on task, asked the right questions, and completed the required tasks in a timely fashion! Strong work team!

CEO, SDOH2Health LLC

Mindbowser was easy to work with and hit the ground running, immediately feeling like part of our team.

CEO, Stealth Startup

Mindbowser was an excellent partner in developing my fitness app. They were patient, attentive, & understood my business needs. The end product exceeded my expectations. Thrilled to share it globally.

Owner, Phalanx

Mindbowser's expertise in tech, process & mobile development made them our choice for our app. The team was dedicated to the process & delivered high-quality features on time. They also gave valuable industry advice. Highly recommend them for app development...

Co-Founder, Fox&Fork
