Behavioral health is one of the fastest-growing areas of telehealth adoption, yet it is also the most vulnerable to privacy risks. Unlike general medical encounters, therapy sessions often surface information about trauma, substance use, and family relationships that is deeply personal. Patients trust providers to safeguard this data with the highest standards of confidentiality. That trust can be broken instantly if a platform falls short on HIPAA compliance.
For healthcare leaders, the question is no longer whether telehealth can scale behavioral health services, but whether the platform you choose is built to withstand the regulatory, reputational, and technical demands of this field. This is where HIPAA compliance moves from being a regulatory checkbox to becoming the backbone of sustainable behavioral health delivery.
Behavioral health records go beyond lab results or vitals. They include therapy notes that may reveal traumatic experiences, details about substance use, or complex family dynamics. A breach of this kind of information can cause stigma, discrimination, or long-term harm. Protecting these records is not just about following regulations but about honoring the vulnerability patients bring to each session.
Trust is everything in behavioral health. Patients are more likely to delay care or disengage if they suspect their data is not secure. A single headline about a breach can undo years of effort in building credibility. For health systems and digital health companies, reputational damage translates directly into lower adoption and higher dropout rates.
HIPAA violations in behavioral health are costly. The Office for Civil Rights (OCR) has issued multimillion-dollar fines for compliance lapses, especially where sensitive health data was exposed online. Class-action lawsuits often follow, adding financial and operational strain. Payers may also pull back from contracts if a partner shows patterns of weak compliance.
The Privacy Rule requires that only the information needed to deliver care be shared. For behavioral health, this means a platform must allow providers to restrict access to sensitive notes, prevent oversharing in group sessions, and carefully manage data when coordinating with outside specialists. A compliant system ensures that therapists can document care while limiting exposure of unnecessary details to staff who do not need them.
The Security Rule sets clear expectations for how electronic health data must be protected. For telehealth platforms, this includes encryption of all video, chat, and file exchanges both in transit and at rest. Access should be limited through role-based controls, and clinicians should be required to log in using multifactor authentication. Platforms must also generate and store audit logs that track who accessed records and when. These safeguards are not optional in behavioral health, where the risk of misuse or breach is particularly high.
Under the Breach Notification Rule, organizations must promptly notify patients, regulators, and sometimes the media if protected health information is compromised. A telehealth vendor that cannot detect, report, and document breaches creates unacceptable risk for providers. Leaders should confirm that any platform under consideration can generate breach reports and escalate incidents within the required timelines.
Any vendor that handles protected health information on behalf of a provider is considered a business associate under HIPAA. This means telehealth platforms, cloud storage providers, and even messaging tools must sign a BAA. The agreement transfers shared responsibility for compliance and outlines the vendor’s obligations around data use, breach response, and audits. Without a signed BAA, even a technically secure platform cannot be considered HIPAA compliant.
HIPAA applies equally to synchronous video sessions and asynchronous messaging. Behavioral health practices often use secure messaging for follow-up questions, prescription refills, or between-session support. These communications must meet the same standards as live video visits. Leaders evaluating platforms should verify that every communication channel, not just video conferencing, is built to HIPAA standards.
Related read: Streamlining Behavioral Healthcare with Epic EHR Integration: Enhancing Efficiency and Patient Care
Behavioral health patients are often more cautious about sharing personal information than those seeking other types of care. When a platform demonstrates HIPAA compliance, patients gain confidence that their disclosures remain private. This trust translates into stronger engagement, more frequent use of telehealth sessions, and lower no-show rates. In a field where dropout is a constant challenge, compliance directly supports continuity of care.
Providers are more willing to document detailed notes and share information across care teams when they know the system is secure. HIPAA-compliant platforms reduce the fear of accidental disclosure, allowing psychiatrists, therapists, and primary care physicians to collaborate with confidence. This collaboration is particularly important for patients with complex needs who may be navigating both behavioral and physical health conditions.
Payers increasingly require proof that telehealth platforms are HIPAA compliant before they approve contracts or reimburse for services. Compliance ensures that documentation meets both regulatory and interoperability standards, reducing claim denials and delays. For behavioral health organizations operating under tight budgets, faster and more reliable reimbursement has a direct impact on financial sustainability.
A compliant platform ensures that sensitive information can be shared securely between different care settings. For example, a patient moving from outpatient therapy to inpatient care can have records transferred without exposing them to unnecessary risk. HIPAA compliance also facilitates smoother handoffs between psychiatrists, therapists, and primary care providers, resulting in a more integrated care experience for patients.
One behavioral health network significantly expanded its telehealth services only after demonstrating full HIPAA compliance to its payers. Once compliance safeguards were in place, the organization secured new payer partnerships, expanded its digital therapy programs, and improved patient adoption. The lesson is clear: compliance is not only about avoiding penalties but also about unlocking growth opportunities.
Related read: Best Telemedicine Software: Top 10 Platforms for Virtual Healthcare
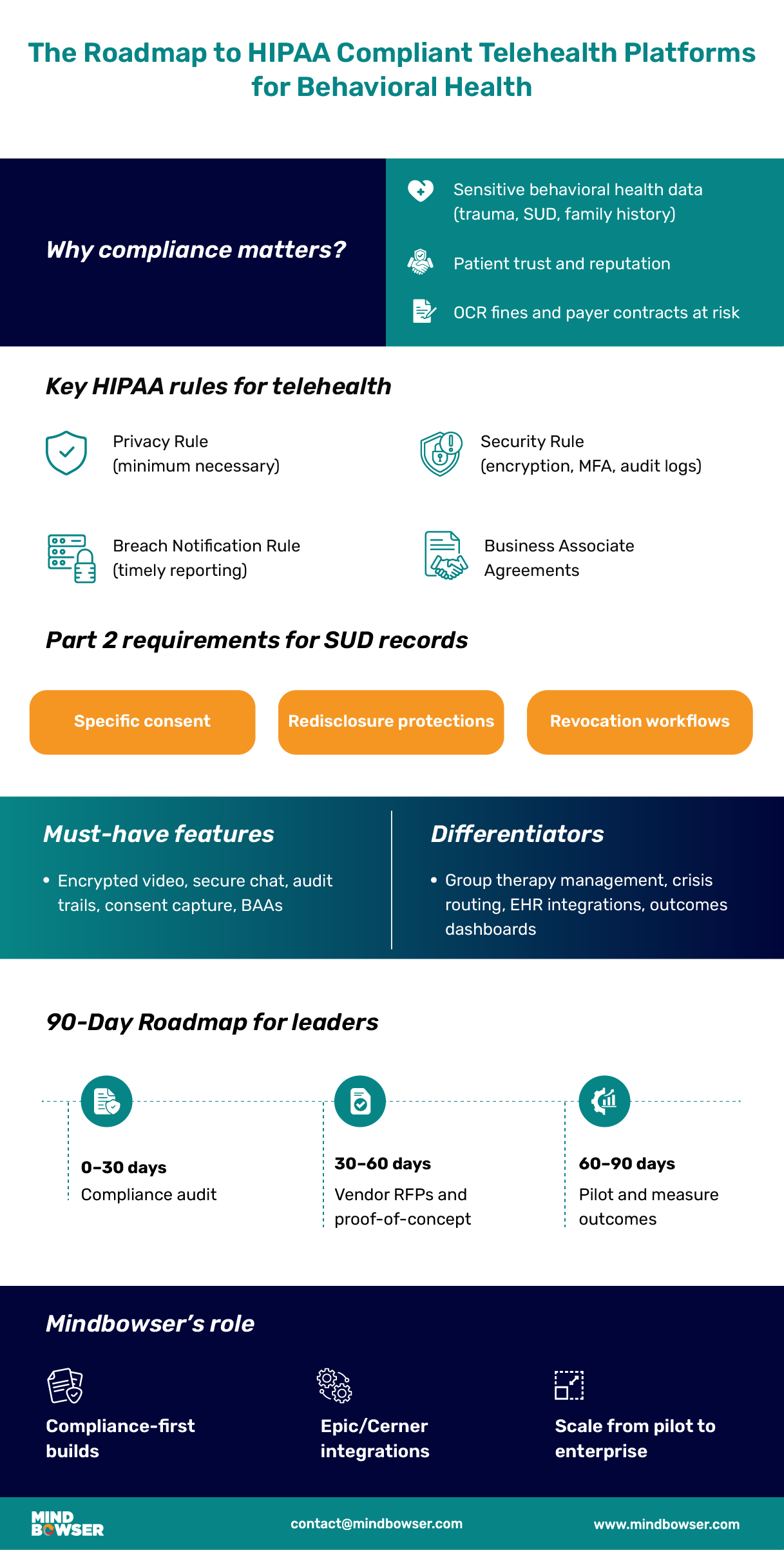
Encrypted video and messaging: Every session, message, and file transfer must be encrypted both in transit and at rest. This prevents unauthorized access even if data is intercepted.
HIPAA-ready file storage: Notes, intake forms, and assessments need secure storage that supports access control and regular audits.
E-signatures: Digital consent forms and treatment agreements should be captured in a secure, legally valid format.
Guardian and parental consent: Platforms must handle situations where minors need caregiver approval to begin therapy. This requires flexible workflows for multiple signers.
42 CFR Part 2 compliance: Substance use disorder records carry additional restrictions beyond HIPAA. Platforms must support specific consent for SUD records and ensure redisclosure rules are enforced.
Revocation workflows: Patients must have the ability to revoke consent, and systems should immediately update access rights to reflect this change.
Controlled visibility: Not every staff member should have access to therapy notes. A compliant platform provides different access levels for clinicians, administrators, and support staff.
Audit trails: Leaders should be able to see exactly who accessed records, what was viewed, and when it happened.
User authentication: Multifactor authentication reduces the risk of unauthorized logins, especially in remote environments.
EHR connectivity: Behavioral health providers using Epic, Cerner, or specialty EHRs need platforms that integrate without compromising security.
Labs and e-prescriptions: Secure orders and prescriptions must be transmitted directly from the telehealth platform to the relevant systems.
Billing and claims: Integration with RCM systems reduces manual errors and ensures that compliant documentation reaches payers quickly.
Compliance logs: Platforms should generate reports that can be shared with regulators or payers on demand.
Incident tracking: Every failed login attempt, unauthorized access, or unusual activity must be recorded.
Performance dashboards: Compliance reporting should also help organizations improve workflows, not just satisfy audits.
Build Your HIPAA-Compliant Telehealth Platform Today
Many generic telehealth platforms advertise themselves as “HIPAA compliant,” but closer review often reveals gaps. Some vendors provide encryption but refuse to sign Business Associate Agreements, which makes their use non-compliant in practice. Others lack features such as consent management and audit trails, which are critical in behavioral health. Leaders should not take compliance claims at face value and must verify each safeguard against HIPAA and 42 CFR Part 2 requirements.
Off-the-shelf tools often store patient data in proprietary systems, making it difficult to export records if an organization switches vendors. This creates long-term risk for providers who may face higher costs or service disruptions if a platform goes out of business or changes terms. Behavioral health organizations require solutions that enable secure data portability, allowing for both compliance and operational flexibility.
General telehealth platforms are usually designed for primary care or urgent care visits. They rarely address the unique needs of behavioral health, such as group therapy management, intensive outpatient programs, or family counseling sessions. These workflows involve multiple participants, sensitive consents, and extended treatment plans that standard video conferencing tools cannot handle. Without customization, providers are left with manual workarounds that increase the risk of non-compliance.
Substance use disorder records are subject to stricter privacy protections than other behavioral health data. Platforms that are not designed with redisclosure rules or consent revocation in mind leave providers exposed to significant legal liability. Even if a tool satisfies HIPAA requirements, it may still fail when it comes to Part 2 compliance. Behavioral health leaders should ensure that any platform in use is explicitly designed to meet both sets of regulations.
Zoom for Healthcare is often used as an entry-level solution for telehealth. While it provides encrypted video conferencing and can sign a BAA, it does not natively support features like consent management, redisclosure controls, or integration with behavioral health EHRs. Custom-built solutions, on the other hand, can embed these requirements directly into the workflow. The difference highlights why behavioral health organizations must carefully weigh the limitations of off-the-shelf options against the long-term benefits of platforms designed for their specific needs.
Mindbowser specializes in developing telehealth platforms that reflect the realities of behavioral health practice. This means designing for cognitive behavioral therapy, dialectical behavior therapy, intensive outpatient programs, and group counseling. Features such as multi-participant session management, secure breakout rooms, and structured digital intake are included from the start. These capabilities ensure that therapy models are not forced into one-size-fits-all technology.
Our development approach embeds HIPAA and 42 CFR Part 2 compliance at every stage of platform design. From how data is captured during intake to how it is shared during care transitions, compliance is not an afterthought but a foundation. We implement role-based access, encryption, consent capture, and redisclosure safeguards as part of the core architecture. This reduces the risk of costly retrofits later and helps organizations remain audit-ready.
Behavioral health organizations rarely operate in isolation. They rely on interoperability with Epic, Cerner, or specialty behavioral health EHRs. Mindbowser has delivered secure integrations for scheduling, encounter notes, lab results, and billing. By building around established interoperability standards, such as FHIR and HL7, we ensure data moves seamlessly between systems while maintaining privacy.
We design platforms that can start small and grow with the organization. A pilot program in one clinic can be scaled to a statewide behavioral health network without rewriting the foundation. Cloud-native architecture, flexible user management, and automated compliance reporting allow leaders to expand services without compromising on privacy or performance.
Mindbowser partnered with a children’s behavioral health network that was struggling with high emergency room utilization. We built a HIPAA-compliant telehealth platform tailored to pediatric therapy, with secure messaging, guardian consent workflows, and integration to the organization’s EHR. Within the first year of launch, the network reported a 30 percent reduction in unnecessary ER visits, along with improved patient satisfaction scores. This example shows the impact of a platform designed with compliance and behavioral health in mind.
Mindbowser is not a product company offering pre-packaged tools. We are a trusted development partner for healthcare organizations that need secure, compliant, and scalable telehealth platforms. By combining domain expertise in healthcare with a track record of HIPAA and Part 2 builds, we help behavioral health leaders move from compliance risk to compliance confidence.
Evaluate your current telehealth platform against HIPAA Privacy, Security, and Breach Notification Rules. Look for encryption, audit logs, access control, and breach reporting functions.
Check for 42 CFR Part 2 readiness if your organization provides substance use disorder services. This includes consent capture, redisclosure restrictions, and revocation workflows.
Identify technology gaps such as missing BAAs, use of third-party tracking tools, or lack of role-based access. These gaps represent immediate risks that need addressing before scaling further.
Buy standard tools for commodity functions like secure video conferencing and basic messaging, where HIPAA compliance is already well supported.
Build custom features for behavioral health-specific workflows such as group therapy management, guardian consent, and redisclosure compliance. These areas require specialized development.
Weigh total cost of ownership by considering not just upfront vendor fees but also long-term flexibility, integration needs, and the cost of retrofitting compliance later.
Demand BAAs from all vendors, including cloud storage, messaging, and analytics partners. Without a signed BAA, you remain exposed to liability.
Test redisclosure handling during proof-of-concept trials. A platform that cannot restrict access to Part 2 records is not viable for behavioral health.
Assess integration readiness with your EHR and billing systems. Vendor claims of “interoperability” should be verified in real use cases, not marketing slides.
Launch a limited pilot that includes intake, therapy sessions, and documentation. Use this to validate compliance controls and gather clinician feedback.
Track metrics such as no-show rates, patient satisfaction, and claim acceptance during the pilot. Use the results to refine workflows.
Scale in phases to avoid overloading teams and to ensure compliance processes remain consistent across multiple clinics or regions.
| Timeline | Action | Outcome |
|---|---|---|
| First 30 Days | Conduct HIPAA and 42 CFR Part 2 compliance audit | Identify platform gaps and immediate risks |
| 30–60 Days | Issue RFPs and run proof-of-concept tests with compliance checks | Shortlist vendors or finalize custom-build plan |
| 60–90 Days | Launch pilot with BAAs signed, redisclosure workflows in place, and integration tested | Validate compliance and ROI before scaling |
Providers who strive for fewer denials, faster recoveries, and long-term financial stability choose custom denial management solutions that align with their workflows and growth.

HIPAA compliance in behavioral health telehealth is essential not just to meet regulatory requirements but to build and maintain patient trust. Behavioral health data is highly sensitive, and platforms must protect therapy notes, substance use records, and personal histories to ensure confidentiality and confidence. Without proper safeguards, patient engagement and continuity of care can suffer.
Investing in a HIPAA-compliant platform also directly impacts clinical adoption and operational efficiency. Features like secure consent management, role-based access, and EHR integration streamline workflows while minimizing legal and reputational risk. Compliance becomes more than a checklist—it supports better outcomes, smoother payer reimbursements, and scalable growth for behavioral health organizations.
Partnering with a platform provider like Mindbowser ensures that behavioral health practices get tailored solutions built for compliance, scalability, and real-world therapy workflows. From group therapy and IOP programs to seamless integration with Epic and Cerner, these solutions allow organizations to expand telehealth services confidently. Ultimately, compliance-first platforms empower both providers and patients to engage in secure, effective, and trusted care.
Yes. All communications, notes, and shared files in group sessions must be encrypted, access-controlled, and auditable. Participants must also be clearly informed of privacy rules before sessions begin.
42 CFR Part 2 places additional requirements on substance use disorder records. A telehealth platform must capture specific patient consent for sharing these records, prevent unauthorized redisclosure, and support consent revocation workflows.
Non-compliance can result in fines from the Office for Civil Rights, class-action lawsuits, payer contract losses, and significant reputational damage. These costs often far exceed the investment required to build or buy a compliant platform.
Generic telehealth tools may cover basic HIPAA requirements, but often fail to support behavioral health-specific workflows, such as family counseling or intensive outpatient programs. A custom platform ensures compliance while also meeting the unique needs of providers and patients.

We worked with Mindbowser on a design sprint, and their team did an awesome job. They really helped us shape the look and feel of our web app and gave us a clean, thoughtful design that our build team could...


The team at Mindbowser was highly professional, patient, and collaborative throughout our engagement. They struck the right balance between offering guidance and taking direction, which made the development process smooth. Although our project wasn’t related to healthcare, we clearly benefited...

Founder, Texas Ranch Security

Mindbowser played a crucial role in helping us bring everything together into a unified, cohesive product. Their commitment to industry-standard coding practices made an enormous difference, allowing developers to seamlessly transition in and out of the project without any confusion....

CEO, MarketsAI

I'm thrilled to be partnering with Mindbowser on our journey with TravelRite. The collaboration has been exceptional, and I’m truly grateful for the dedication and expertise the team has brought to the development process. Their commitment to our mission is...

Founder & CEO, TravelRite

The Mindbowser team's professionalism consistently impressed me. Their commitment to quality shone through in every aspect of the project. They truly went the extra mile, ensuring they understood our needs perfectly and were always willing to invest the time to...

CTO, New Day Therapeutics

I collaborated with Mindbowser for several years on a complex SaaS platform project. They took over a partially completed project and successfully transformed it into a fully functional and robust platform. Throughout the entire process, the quality of their work...

President, E.B. Carlson

Mindbowser and team are professional, talented and very responsive. They got us through a challenging situation with our IOT product successfully. They will be our go to dev team going forward.

Founder, Cascada

Amazing team to work with. Very responsive and very skilled in both front and backend engineering. Looking forward to our next project together.
Co-Founder, Emerge

The team is great to work with. Very professional, on task, and efficient.

Founder, PeriopMD

I can not express enough how pleased we are with the whole team. From the first call and meeting, they took our vision and ran with it. Communication was easy and everyone was flexible to our schedule. I’m excited to...

Founder, Seeke

We had very close go live timeline and Mindbowser team got us live a month before.

CEO, BuyNow WorldWide

Mindbowser brought in a team of skilled developers who were easy to work with and deeply committed to the project. If you're looking for reliable, high-quality development support, I’d absolutely recommend them.

Founder, Teach Reach

Mindbowser built both iOS and Android apps for Mindworks, that have stood the test of time. 5 years later they still function quite beautifully. Their team always met their objectives and I'm very happy with the end result. Thank you!

Founder, Mindworks

Mindbowser has delivered a much better quality product than our previous tech vendors. Our product is stable and passed Well Architected Framework Review from AWS.

CEO, PurpleAnt

I am happy to share that we got USD 10k in cloud credits courtesy of our friends at Mindbowser. Thank you Pravin and Ayush, this means a lot to us.

CTO, Shortlist

Mindbowser is one of the reasons that our app is successful. These guys have been a great team.

Founder & CEO, MangoMirror

Kudos for all your hard work and diligence on the Telehealth platform project. You made it possible.

CEO, ThriveHealth

Mindbowser helped us build an awesome iOS app to bring balance to people’s lives.

CEO, SMILINGMIND

They were a very responsive team! Extremely easy to communicate and work with!

Founder & CEO, TotTech

We’ve had very little-to-no hiccups at all—it’s been a really pleasurable experience.

Co-Founder, TEAM8s

Mindbowser was very helpful with explaining the development process and started quickly on the project.

Executive Director of Product Development, Innovation Lab

The greatest benefit we got from Mindbowser is the expertise. Their team has developed apps in all different industries with all types of social proofs.
Co-Founder, Vesica

Mindbowser is professional, efficient and thorough.

Consultant, XPRIZE

Very committed, they create beautiful apps and are very benevolent. They have brilliant Ideas.

Founder, S.T.A.R.S of Wellness

Mindbowser was great; they listened to us a lot and helped us hone in on the actual idea of the app. They had put together fantastic wireframes for us.

Co-Founder, Flat Earth

Mindbowser was incredibly responsive and understood exactly what I needed. They matched me with the perfect team member who not only grasped my vision but executed it flawlessly. The entire experience felt collaborative, efficient, and truly aligned with my goals.

Founder, Child Life On Call

The team from Mindbowser stayed on task, asked the right questions, and completed the required tasks in a timely fashion! Strong work team!

CEO, SDOH2Health LLC

Mindbowser was easy to work with and hit the ground running, immediately feeling like part of our team.

CEO, Stealth Startup

Mindbowser was an excellent partner in developing my fitness app. They were patient, attentive, & understood my business needs. The end product exceeded my expectations. Thrilled to share it globally.

Owner, Phalanx

Mindbowser's expertise in tech, process & mobile development made them our choice for our app. The team was dedicated to the process & delivered high-quality features on time. They also gave valuable industry advice. Highly recommend them for app development...

Co-Founder, Fox&Fork
